No woman should die from cervical cancer. Yet, it is the second leading cancer and significant contributor to cancer-related deaths in Indian women. Despite being one of the most preventable and curable cancers, if detected early, the cervical screening rate in India is dismal at 2%. A vaccine for cancer is now available but its price puts it out of reach for many. The inequities in cervical cancer screening, prevention and treatment along with its high mortality and morbidity make it an important public health problem not only for India but also globally.
Also Read:Indigenous HPV vaccine, the rhetoric and the reality
Every January is Cervical Cancer Awareness Month. In addition to the discussion about its causes and risk factors, this piece aims to spark dialogue among public health advocates, policymakers, and readers about the urgent need for equitable cervical cancer prevention. It underscores the importance of bridging the gap to ensure every woman, regardless of income, has the opportunity to protect herself from this preventable disease.
The cervix is the entrance to the uterus from the vagina, it is anatomically part of the female reproductive tract. The most common viral infection of this body part is caused by Human Papilloma Virus (HPV), which causes almost 99% of cervical cancers. While most HPV infections are asymptomatic and cleared by the immune system within a few months to years, persistent infection with high-risk HPV types can lead to cervical cancer.
Symptoms of early-stage cervical cancer include vaginal bleeding post intercourse and menopause, between periods or heavier or longer periods and, strong-odored and watery vaginal discharge. Advanced cervical cancer symptoms include difficulty or pain in bowel movement and urination, abdominal pain and swelling in legs. Since these symptoms overlap with other health conditions, seeking professional health consultation is essential.
Apart from cervical cancer, HPV infection is also associated with cancers of the head, neck, oropharynx and anogenital area and anogenital warts. Rarely, warts form on the larynx and other parts of the respiratory tract. While HPV infection is more common in women, this virus is also prevalent in men.
Several factors increase the risk of HPV infection including unsafe sexual contact, multiple sexual partners, age at first sexual intercourse along with education and literacy levels, and a weakened immune system resulting from various reasons such as HIV infection or smoking.
With over 200 HPV types, these can be high or low risk based on their potential to cause cancer. Currently twelve HPV types are identified as high-risk (oncogenic), and causing cancer in humans. HPV16 and 18 are most oncogenic and also the most common type found in regions of high prevalence globally, including India.
As per the World Health Organization (WHO), screening, prophylactic vaccination against HPV, and treatment of precancerous lesions are effective strategies to prevent cervical cancer.
Precancers are often asymptomatic, requiring regular screening even post-vaccination. While cervical cancer screening is recommended every 5-10 years starting age 30, women with HIV should get screened every 3 years starting age 25. The three main methods of screening are HPV test, Pap smears and HPV/Pap co-test.
The HPV test checks for HPV infection. Last year, the US FDA approved HPV self-collection. In India, several companies have started offering HPV at-home screening tests priced around Rs. 2500 – Rs. 3000. On the other hand, Pap smear test collects cervical cells to detect presence of precancerous and cervical cancer cells. A Pap smear costs around Rs. 500. The HPV/Pap co-test checks for both and costs around Rs. 3000 – Rs. 4000.
Vaccination is central to the WHO Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Problem. Implementing this strategy could prevent 60 million cervical cancer cases and 45 million deaths over the next 100 years. Being vaccinated between ages 9 – 14 years, before any exposure to HPV, is highly effective in preventing the infection. Hence, vaccination is not recommended in sexually active adults, who may already have been exposed to HPV.
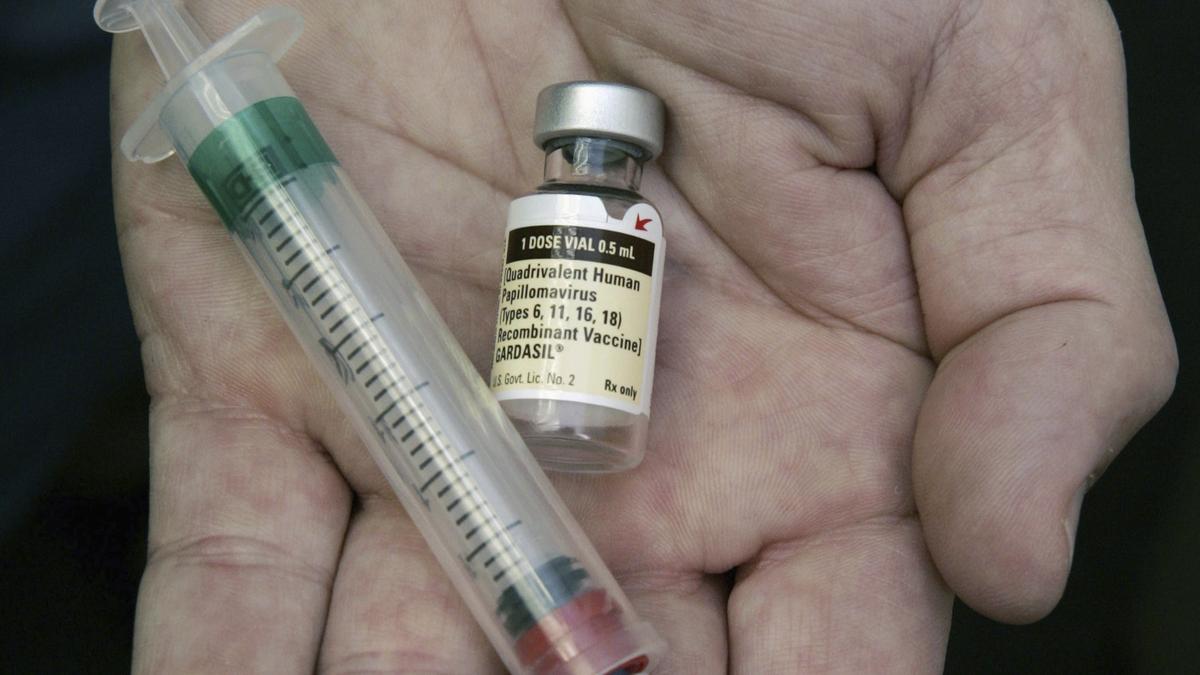
There are six licensed HPV vaccines: three bivalent, two quadrivalent, and one nonavalent, all globally marketed. Valency refers to the number of virus types against which the vaccine is effective. All of these vaccines effectively prevent HPV types 16 and 18, responsible for 70% of cervical cancer cases, and associated precancerous lesions. The quadrivalent vaccine also protects against anogenital warts caused by HPV types 6 and 11, while the nonavalent vaccine adds coverage for types 31, 33, 45, 52, and 58. Clinical trials and global surveillance confirm their safety and efficacy.
As per the December 2022 WHO Position on HPV vaccines, a one- or two-dose schedule is recommended for girls aged 9 – 14 and women aged 15 – 20. For women over 21, two doses with a six-month interval are advised. Immunocompromised individuals, including those with HIV, require a minimum of two doses, with three doses recommended when feasible.
While HPV vaccines are a powerful preventive tool, their high cost – INR 4,000 to INR 11,000 per dose – makes them inaccessible to millions of women, especially those in rural, low-income backgrounds and underserved areas. Neither is it part of the National Immunisation Programme. Essentially, lack of equitable access to a life-saving intervention is exacerbating health inequities in cervical cancer.
In India, there is a high correlation between literacy levels and cervical cancer. Hence, in the absence of affordable vaccines, alternative strategies and investment in public health education aimed at health behavior change becomes crucial. Specifically, education on the importance of screening, managing anxiety about screening and safe sexual practices are important measures. To improve the efficacy of education, involving men in the campaign is an important aspect of public health education. These measures can serve as vital stopgaps until vaccines are made accessible to all.
(Dr. Vid Karmarkar is the founder of Canseva Foundation, which is on a mission to reduce financial toxicity in cancer care. vid.karmarkar@gmail.com)
Published – January 12, 2025 02:11 pm IST