Sleep has long been recognised as an active process by the scientific community, contrary to the popular belief of it being a period of inactivity. Sleep is defined as a normal, reversible, recurring state of reduced responsiveness to external stimulation and relative physical immobility.
Understanding the functions of sleep is crucial to understanding the consequences of sleep-deprivation and sleep-related disorders. The functions of sleep include: fostering optimal brain growth and development; enhancing learning, attention and memory; regulating emotions, appetite and decision-making; strengthening of the immune functions as well as optimal time for rest and repair of body tissues.
The composition and functions of sleep vary with age and development. The changes noted with increasing age from infancy to adulthood are a decrease in total sleep time and the gradual setting up of a consistent sleep-wake cycle. Sleep health is a topic that has just recently garnered worldwide interest in scientific circles; however, this is yet to make much headway amongst the general public. There has also been a much-needed shift in importance from ‘treatment of insomnia’ to ‘prevention of sleep disorders and maintenance of good sleep health’.
The array of consequences of sleep disruption range from irritability to poor academic and work performance to being triggers for major mental illnesses and suicides. The impact of these are equally (if not more) significant in children and adolescents as in adults. Sleep disorders in children have ramifications in three aspects: the sleep disorder in itself and the distress due to it; the long-term impacts it has on the child’s or adolescent’s academics, schooling, physical activity, emotional regulation, risk-taking behaviour and effect on comorbid illnesses which could be physical or mental and the impact of family behaviour on the child’s sleep and vice- versa.
The burden among children
Let us see what the statistics say about paediatric sleep disorders. Around 80% of the child and adolescent population worldwide have sleep disorders or complaints related to sleep. Persistent sleep difficulties in childhood predict psychiatric problems in adult life and sleep deprivation also increases health complaints in children. Crucially, parental stress related to the behavioural problems in sleep-deprived children can affect their mental and/or physical well being
There are two main types of sleep disorders: primary sleep disorders and secondary sleep disorders, which have consequences of physical or mental illnesses or drug abuse. Primary sleep disorders seen in child and the adolescent population present in various forms. Insomnia, which is defined as persistent reduction in total sleep duration or poor quality of sleep is one. Hypersomnia, which is an increase in sleep duration is another. Parasomnias are undesirable physical events or experiences that occur during entry into sleep, within sleep or during arousal from sleep. There are also sleep-related breathing disorders and sleep-related movement disorders like restless leg syndrome and nocturnal teeth grinding. This apart, there are disorders of the sleep-wake cycle. All these conditions impact sleep in terms of duration and /or quality of sleep.
What is insomnia?
Insomnia can present in the form of difficulty in falling asleep, bedtime resistance, frequent nighttime awakenings, imposed sleep restrictions, unrefreshed sleep and /or poor sleep hygiene persisting over three months
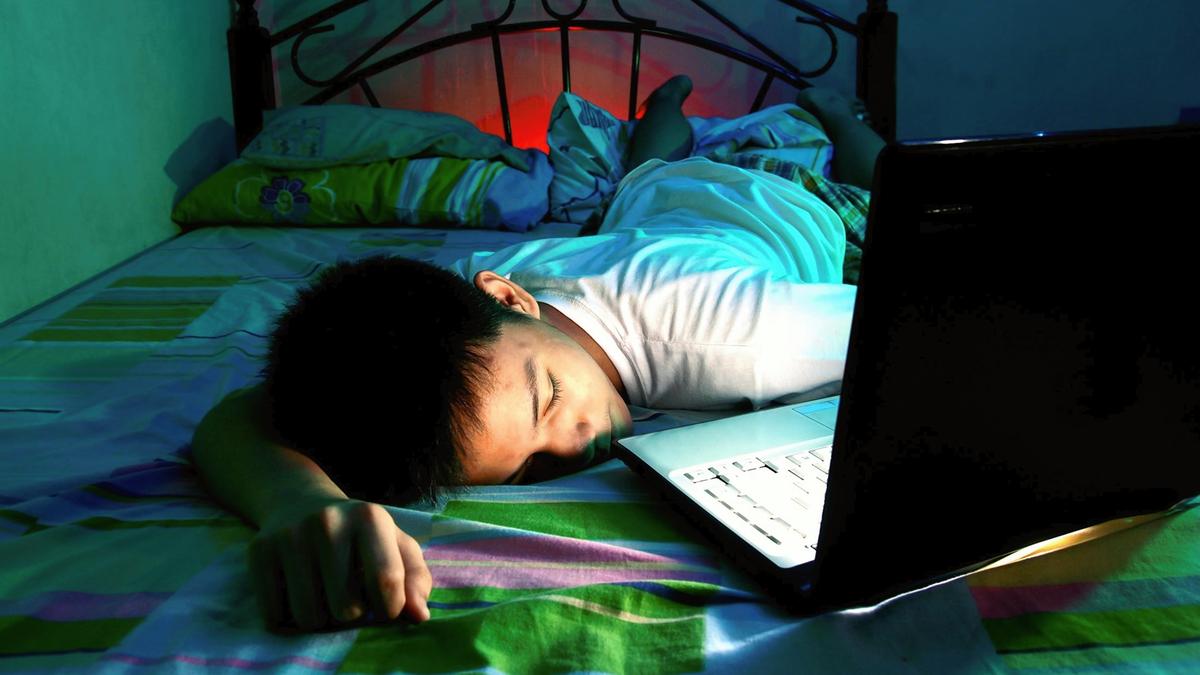
The risk factors for insomnia include: predisposition to mental or physical illnesses; stressors like difficult home or family situations, safety concerns or domestic abuse; poor limit-setting by parents which may cause bedtime stalling or refusal; environmental factors like cramped sleeping conditions, lack of a conducive temperature; sleep difficulties or poor sleep hygiene in parents and excessive use of technology especially in the form of screens
Strategies that can be implemented by family members to help the child with insomnia include identifying the stressors; try to eliminate or alleviate them and initiate good sleep habits.

Sleep hygiene is a set of practices that helps individuals sleep better. These include creating conducive and optimal bedroom or bedtime conditions; restriction of screens, beverages and water intake a few hours prior to bedtime; maintaining consistent bedtime routine; a consistent sleep schedule; regular physical activity; restriction of daytime naps and most importantly, role-modelling healthy sleep habits.
If the symptoms of insomnia persist or continue to be problematic, it is best to to consult a pediatric sleep expert at the earliest.
What is obstructive sleep-disordered breathing?
This disorder is characterised by snoring and laboured breathing due to a partial blockage of the air passages within the body. The symptoms include nighttime snoring, excessive daytime sleepiness, bedwetting, morning headaches, restless sleep and irritability during the day. The obstruction of the air passages in children is commonly due to tonsils or adenoid enlargement or obesity.
The risk factors for this disorder include obesity, exposure to passive cigarette smoke and poor air quality. Steps that can be taken by parents include measures to alleviate risk factors and a consultation with an expert.
What is a nightmare disorder?
This is a type of parasomnia where the child has frequent, vivid and distressing dreams, which often result in awakenings. This disorder is usually the result of a stress in the form of a recent psychosocial issue or a major event that may even lead to diagnosis of post-traumatic stress disorder (PTSD).
Family members can do quite a bit to help these children by consistently reassuring the child, avoiding negative associations or responses to the symptoms, encouraging sleep hygiene especially by restricting TV viewing before bedtime. They can also help by re-scripting or reframing the content/plot of the nightmare. Rarely, such children may require therapy and medication.

What is sleep enuresis?
Sleep enuresis or bedwetting is considered normal from infancy up until toddlerhood. However =, its persistence after the age of five years qualifies for a diagnosis and needs medical attention. In some cases, children who may have been previously dry by night (for more than 6 months ) may resume bedwetting , and this is called secondary enuresis. This disorder is more frequently seen in girls than boys until the age of 11. This disorder is also highly under-reported due to social stigma and a lack of awareness.
The risk factors for this illness include a history of similar symptoms in parents, urinary tract infections, excessive evening fluid intake and stress in the form of parental divorce, neglect, physical and/or sexual abuse. the psychological consequences of bedwetting range from self-esteem issues, feelings of guilt and shame, social anxiety and isolation, frequent nighttime awakenings, depressive symptoms and significant family conflicts.
Parental strategies for managing bed-wetting start with understanding and recognising the problem followed by help-seeking. This step is often the most crucial and decisive in the management of this problem. The next steps would be: forming a plan, in collaboration with the child, for reduction of fluids before bedtime , encouraging daytime urination, preventing daytime restriction of urination (a malady frequently seen in young girls wanting to avoid public toilets) , avoiding negative responses to the symptoms and refraining from punishments.
Parents can also instate an alarm system by which the child is encouraged to use the toilet during bed hours. As we can see, the steps require a lot of effort and dedication from the parents; however the results have been shown to be rewarding.
Last but not the least, seek professional help when the symptoms begin to interfere with the child’s day-to-day functioning.
Sleep disorders secondary to psychiatric disorders
Sleep is frequently disrupted in children with psychiatric disorders and neurodevelopmental disorders. Anxiety and depressive disorders are commonly associated with delays in sleep onset and frequent nighttime awakenings, sometimes with nightmares. Restlessness and bedtime tantrums are frequently seen in children with neurodevelopmental disorders like intellectual disabilities, ADHD and autism. These sleep disorders may resolve with the adequate management of the primary psychiatric diagnosis and relevant therapy. In corollary, improvement in sleep difficulties positively impacts the symptoms of the primary psychiatric disorder.
Sleep disorders secondary to medical conditions
Many physical conditions have profound effects on children’s sleep. Common conditions like gastro- oesophageal reflux disorder (GERD) where a child has the frequent re-entry of stomach content into the oesophagus may disrupt the child’s sleep. Migraines or other pain syndromes affect the onset and maintenance of sleep while seizures may lead to night-time awakenings.
Adequate management of the primary illness helps in reduction of sleep difficulties.
Paediatric sleep health as a branch of medicine is still in its nascent stages, however, raising awareness about this is paramount, and the need of the hour. In this digital era, when forces to disrupt sleep are overwhelming, we must learn to prioritise sleep and instil healthy sleep habits in our children, who are our future.
(Dr. Maria Antony is a specialist in child and adolescent mental health. mariaantonycmc@gmail.com)
Published – December 27, 2024 07:08 pm IST